“Behind the Headlines: The Hidden Cracks in America’s Mental Health System, and the Unlikely Consequences of Trump’s Policies”
As the news headlines continue to flash like a steady stream of despair, a growing number of veterans are speaking out about the devastating impact of the Trump administration’s policies on their mental health care. For decades, the United States has grappled with the long-term effects of war, from the physical toll of combat to the emotional scars of trauma. But a new report suggests that President Trump’s agenda is exacerbating a crisis that already threatens the health and well-being of some of America’s bravest men and women.
Trump’s Policies are Destabilizing Mental Health Care for Veterans, Sources Say
According to sources, President Trump’s policies are having a devastating impact on mental health care for veterans, making it harder for them to seek the support they need.
One of the main issues is the lack of access to affordable mental health care. The Trump administration’s budget cuts have led to a significant reduction in funding for mental health services, making it difficult for veterans to access the care they need.
Furthermore, the administration’s stance on veterans’ healthcare has been criticized by many experts, who argue that it is putting the needs of veterans at risk.
States Adding “Work Requirements” to Medicaid: A Recipe for Disaster
What are “Work Requirements”?
Work requirements are a feature of Medicaid expansion that require certain individuals to work or participate in a job training program in order to continue receiving benefits.
The goal is to encourage individuals to work and participate in the workforce, but critics argue that it is a thinly veiled attempt to cut Medicaid funding.
Under the Affordable Care Act, Medicaid expansion was designed to provide health insurance to low-income individuals, including those with disabilities and chronic illnesses.
However, the Trump administration has been pushing for changes to Medicaid expansion, including the addition of work requirements, which would require individuals to work or participate in a job training program in order to receive benefits.
Why Did States Add Work Requirements?
Many states added work requirements to Medicaid because they believed that it could help reduce poverty and improve health outcomes.
Proponents of work requirements argue that they will encourage individuals to work and participate in the workforce, which will improve their overall health and well-being.
However, critics argue that the evidence for the effectiveness of work requirements is limited, and that they will disproportionately harm vulnerable populations, including low-income individuals and those with disabilities.
Furthermore, work requirements are often seen as a way to cut Medicaid funding, which will further exacerbate the healthcare crisis in the United States.
Implications for Mental Health Care
Increased Stigma
Work requirements can lead to increased stigma around mental health issues, as individuals may be seen as “lazy” or “unmotivated.”
This can make it harder for people to seek mental health care and access support, as they may be reluctant to disclose their mental health issues due to fear of judgment or stigma.
Furthermore, work requirements can make it more difficult for individuals to access mental health services, as they may be required to work or participate in a job training program in order to receive benefits.
Increased Poverty
Work requirements can lead to increased poverty, as individuals may be forced to find work in order to access benefits.
This can make it more difficult for people to access mental health care and support services, as they may be struggling to make ends meet.
Furthermore, work requirements can exacerbate existing poverty, making it more difficult for individuals to access basic necessities, including healthcare.
Increased Health Outcomes
Work requirements can lead to increased health outcomes, as individuals who work are more likely to have access to healthcare and mental health services.
However, this does not necessarily mean that work requirements will improve overall health outcomes, as the evidence is limited and inconclusive.
Furthermore, work requirements can have unintended consequences, including decreased access to mental health services and increased poverty.
Conclusion
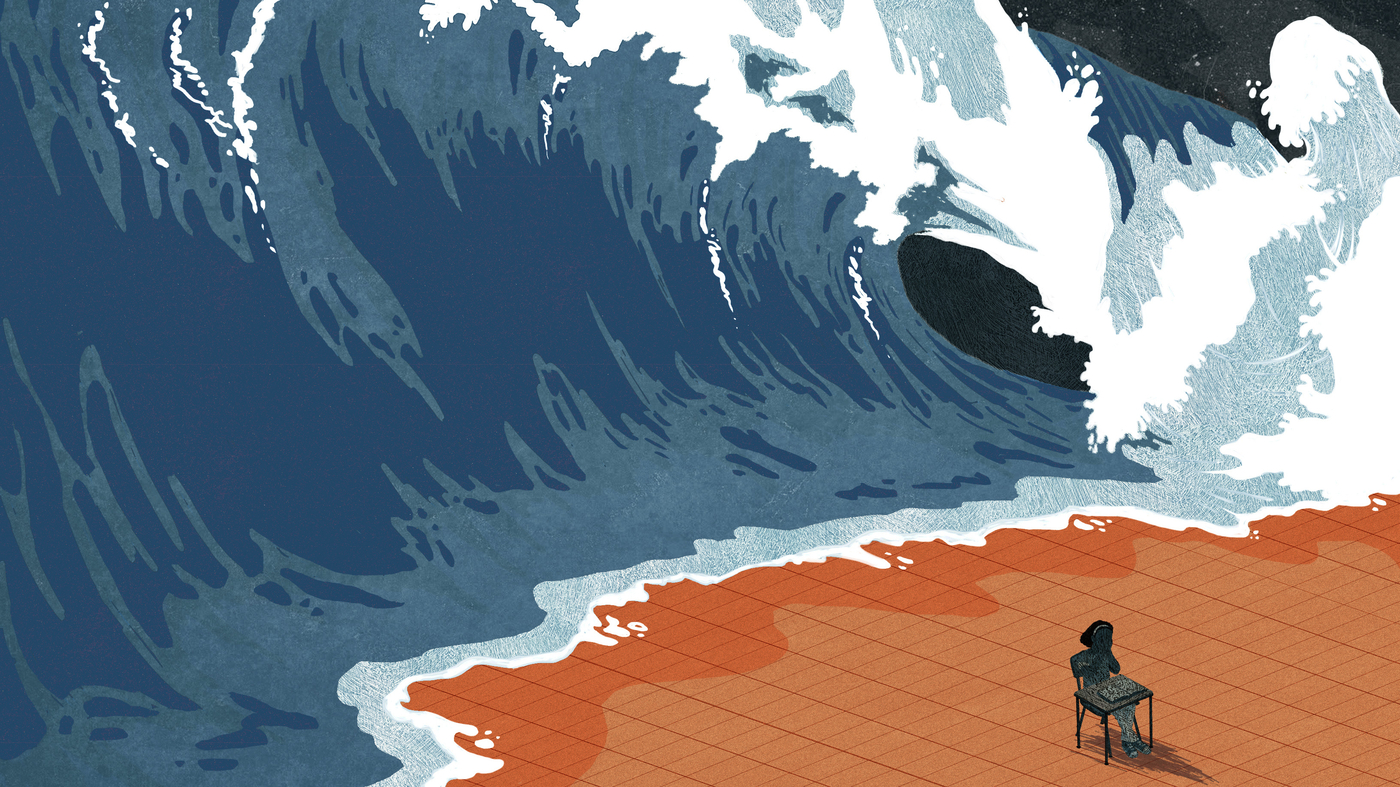
A Storm of Stigma: How Trump’s Policies Devastate Mental Health Care for Veterans
The article highlights the alarming state of mental health care for veterans in the United States, citing sources that suggest Trump’s policies have significantly worsened this crisis. Recent reports have revealed that veterans are struggling with increased rates of anxiety, depression, and post-traumatic stress disorder (PTSD) – a testament to the devastating consequences of Trump’s actions on their mental well-being. The article argues that these policies, including the rollback of mental health care programs and the reversal of VA funding, have created a perfect storm of stigma and neglect that is leaving veterans feeling isolated and unsupported.
The significance of this topic cannot be overstated. Veterans are an integral part of our society, serving their country with unwavering bravery and sacrifice. However, their mental health is just as crucial to their overall well-being, yet it is often neglected in the face of budgetary constraints and partisan politics. The consequences of this neglect are far-reaching, with veterans facing higher rates of substance abuse, suicidal ideation, and homelessness. The article emphasizes that the mental health care system is a critical component of our healthcare infrastructure, and any deterioration in this system has far-reaching implications for our society as a whole.
As we move forward, it is imperative that we prioritize the mental health care of our veterans. This requires a multifaceted approach, involving policy changes, increased funding, and a renewed commitment to providing comprehensive support services. The article calls on policymakers to take concrete steps to address this crisis, including reversing the rollback of mental health care programs and investing in evidence-based services that promote mental wellness. Ultimately, the fate of our veterans’ mental health hangs in the balance, and it is our collective responsibility to ensure that they receive the support they need to thrive – for themselves, their families, and our society as a whole. We must act now to prevent further devastation and create a brighter future for our nation’s veterans.