Imagine a future where damaged brain tissue could be repaired, not with invasive surgery, but with the precise placement of microscopic, self-repairing cells. This isn’t science fiction—it’s the promise of stem cell therapy, and a new hybrid technology is bringing us closer than ever to making it a reality.
Revolutionizing Brain Repair
Stem cell-based brain repair for Parkinson’s disease has long shown promise, but the process has been hindered by the challenges of transplanting induced stem cells.
The current approach involves replacing dead brain cells with induced stem cells, which are reprogrammed from adult cells such as skin cells. These induced stem cells can be converted in the laboratory into the appropriate type of brain cell required for repairing the Parkinson’s brain.
However, these skin cells-turned brain cells need to be transplanted into the brain at a very early stage in their conversion, and the vast majority of the cells do not continue to convert into the mature cells that are required for the therapy to work.
The need for a supportive environment for cell maturation
The key to successful stem cell-based brain repair lies in creating an environment that nurtures and supports the transplanted cells, allowing them to mature and repair the damaged brain tissue.
This is where the collagen hydrogel comes in, providing a supportive environment that dramatically improves cell maturation and reparative ability.
The Breakthrough: Collagen Hydrogel
Neuroscientists at University of Galway have made an exciting discovery that could revolutionize stem cell-based brain repair therapy for Parkinson’s disease.
The team has developed a collagen hydrogel that nurtures, supports, and protects the transplanted cells, dramatically improving their survival and reparative ability.
Introducing the collagen hydrogel
The collagen hydrogel is a game-changing innovation that provides the necessary support and environment for the transplanted cells to mature and repair the damaged brain tissue.
Commenting on the research finding, the lead neuroscientist on the project, Professor Eilís Dowd, explained that “Our hydrogel nurtures, supports and protects the cells after they are transplanted into the brain, and this dramatically improves their maturation and reparative ability.
The Michael J. Fox Foundation awarded $300,000 to continue the development of the hydrogel, with the aim of understanding how the immune system in the brain reacts when cells are transplanted alone versus when they are transplanted in combination with the hydrogel.
The Significance of the Hydrogel in Brain Repair Approaches for Parkinson’s Disease
Brain repair for Parkinson’s disease involves replacing the dead cells by transplanting healthy brain cells back into the brain. Recent advancements in regenerative medicine and stem cell technology have made it possible to use induced stem cells as a source of healthy cells. Induced stem cells are reprogrammed from adult cells, such as skin cells, and can be converted in the laboratory into the appropriate type of brain cell required for repairing the Parkinson’s brain.
However, these skin cells-turned brain cells need to be transplanted into the brain at a very early stage in their conversion, and the vast majority of the cells do not continue to convert – once in the brain – into the mature cells that are required for the therapy to work. In work funded by The Michael J. Fox Foundation for Parkinson’s Research (MJFF) and Science Foundation Ireland, published this week in the Journal of Neural Engineering, the team in the College of Medicine, Nursing and Health Sciences at University of Galway have shown that transplanting the immature cells in a collagen hydrogel dramatically improves both their survival and maturation in the brain.
Understanding Immune System Reaction
The research aims to understand how the immune system in the brain reacts when cells are transplanted alone versus when they are transplanted in combination with the hydrogel. The study will investigate the immune system’s response to transplanted cells alone versus cells with hydrogel, and the importance of this research in advancing brain repair therapies.
The Future of Stem Cell Therapy and Beyond
The revolutionary potential of stem cell therapy lies in its ability to integrate with precision medicine, immune modulation strategies, and gene editing advancements. Synergies with bioengineering for personalized regenerative therapies offer a roadmap for the future.
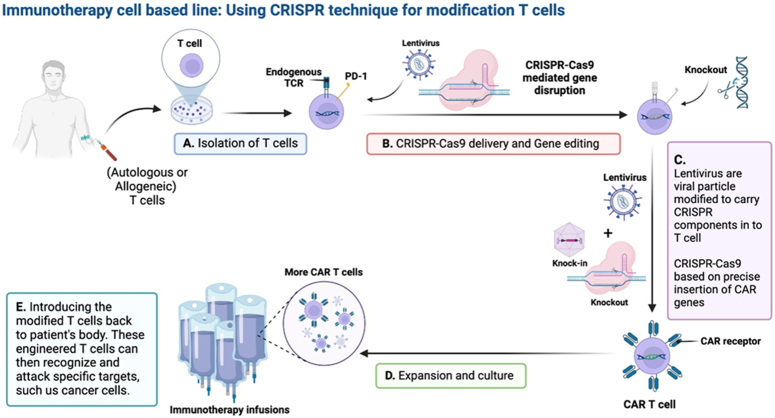
Regulatory considerations for clinical translation are paramount, requiring adherence to strict guidelines and directives to ensure safety and efficacy. The future of stem cell therapy lies in precision medicine integration, immune modulation strategies, advancements in gene editing technologies, and synergies with bioengineering, paving the way for continued evolution and personalized regenerative therapies.
Conclusion
As researchers continue to push the boundaries of stem cell therapy, a groundbreaking new hybrid technology has emerged as a beacon of hope for those suffering from debilitating brain diseases. According to News-Medical, this innovative approach combines the strengths of two distinct methodologies to achieve unprecedented precision in treating neurological conditions. By harnessing the power of both induced pluripotent stem cells (iPSCs) and gene editing tools, scientists have successfully developed a more targeted and effective treatment strategy. This breakthrough has the potential to revolutionize the field of regenerative medicine, offering new avenues for therapy and potentially transforming the lives of millions.
The significance of this achievement cannot be overstated. For individuals grappling with the complexities of Alzheimer’s, Parkinson’s, and other brain disorders, access to effective treatments has long been a pressing concern. The emergence of this hybrid technology offers a glimmer of hope, as it allows researchers to tailor their approaches to address the unique needs of each patient. This targeted approach has the potential to significantly improve treatment outcomes, reducing the risk of adverse effects and minimizing the burden on patients and their families. As this technology continues to evolve, we can expect to see significant advancements in the field of brain disease research, with far-reaching implications for the medical community and beyond.
As we look to the future, it is clear that this hybrid technology represents a major step forward in the fight against brain diseases. With its potential to transform the lives of millions, it is a testament to the power of human ingenuity and the dedication of researchers around the world. As we move forward, it will be essential to continue pushing the boundaries of this technology, exploring new applications and refining existing approaches to maximize its impact. Ultimately, the successful development of this hybrid technology serves as a powerful reminder of the boundless potential of science to heal and transform, and we can only imagine the profound impact it will have on the lives of those who need it most.