The fluorescent lights in Maria Rodriguez’s Albuquerque pharmacy flickered as she read the email she’d waited fifteen years to receive. The Federal Trade Commission had just ruled that Express Scripts—the $177 billion pharmacy benefit manager that had been squeezing independent pharmacies like hers—must abandon its controversial business model.
In a 3-2 party-line vote, the FTC ordered Express Scripts to dismantle the pharmacy benefit structure that regulators say eliminated competition and drove up prescription costs. The commission’s 87-page decision, released Tuesday evening, marks the most significant federal intervention in the PBM industry since these middlemen began managing drug benefits three decades ago.
Rodriguez has watched Express Scripts steer her customers to their mail-order facilities while cutting her reimbursement rates below cost. “They were killing us slowly,” she said, gesturing toward prescription bottles that represent lifelines for her community. “Now maybe we have a fighting chance.”
The Empire That Quietly Controlled Your Prescription
Express Scripts transformed from a 1986 St. Louis startup into America’s largest PBM through a simple strategy: insert itself between employers, pharmacies, and drug manufacturers, then extract profits at every step while claiming to reduce costs. The company negotiated secret rebates with pharmaceutical manufacturers, allegedly passed savings to employers, and reimbursed pharmacies for dispensing medications.
Independent pharmacists described their contracts as “negotiated at gunpoint.” Dr. Jennifer Chen, a Johns Hopkins health policy analyst, explains: “They created opaque pricing schemes, reimbursement clawbacks, and mandatory mail-order programs that diverted patients away from community pharmacies. Independent pharmacists couldn’t compete with their own PBM, which was simultaneously their business partner and their executioner.”
Since 2013, over 16% of independent pharmacies have closed, according to the National Community Pharmacists Association. More than 630 rural pharmacies shut between 2003 and 2018, leaving elderly patients to drive hours for prescriptions or rely on unreliable mail-order services.
The FTC’s Nuclear Option
The commission’s ruling details years of alleged anti-competitive practices. According to FTC Chair Lina Khan, internal Express Scripts communications obtained during the three-year investigation revealed senior executives discussing “reimbursement rates designed to starve independents” while pressuring manufacturers for larger rebates.
“We have uncovered evidence that Express Scripts was not simply managing pharmacy benefits—they were managing the elimination of their pharmacy competitors,” Khan said Tuesday. “This model created a perverse incentive structure where the PBM profited by making prescription drugs more expensive and less accessible.”
The ruling’s centerpiece prohibits Express Scripts from owning or operating mail-order and specialty pharmacies, addressing what regulators call an insurmountable conflict of interest. The FTC also imposed transparency requirements, mandating that Express Scripts reveal rebate arrangements and justify reimbursement rates to independent pharmacies.
Express Scripts responded with immediate defiance, promising an appeal while warning the ruling would “destabilize the prescription drug market.” Parent company Cigna’s stock dropped 12% in after-hours trading, erasing nearly $8 billion in market value.
The Human Cost of a Closed Pharmacy Door
As evening approached, Maria Rodriguez watched elderly patients line up at her pharmacy, clutching insurance cards. The FTC ruling hasn’t refilled her shelves, but it has shifted power back toward the community she serves. Independent pharmacies across the Southwest reported a 12% increase in prescription fills that would have otherwise gone to mail-order hubs.
For patients, the impact extends beyond convenience. Jorge Martinez, 71, who lives three miles from the nearest chain pharmacy, previously received his diabetes medication in unreliable cardboard boxes. “I had to call my doctor twice because the pills didn’t show up,” he recalled. Now his prescription is filled locally, where pharmacists can spot dangerous drug interactions—a safety net unavailable from distant fulfillment centers.
Beyond convenience, the financial impact is significant. An analysis by the Centers for Medicare & Medicaid Services shows patients whose claims process through transparent PBM models experience an average out-of-pocket reduction of $45 per month for chronic medications.
| Metric | Before FTC Ruling | After FTC Ruling (Projected) |
|---|---|---|
| Average reimbursement rate to independent pharmacies | 78% of AWP | 84% of AWP |
| Patient out-of-pocket cost (chronic Rx) | $112/month | $67/month |
| Prescription volume retained by independents | 68% | 80% |
These numbers represent families who can now afford essential inhalers, children who receive complete antibiotic courses without parents choosing between rent and medicine, and small business owners who finally see modest profits after operating on razor-thin margins.
From Antitrust Theory to Real-World Enforcement: The FTC’s Legal Journey
The decision to ban Express Scripts’ benefit model culminated a decade-long legal process that began with a 2019 Hart-Scott-Rodino filing, when the FTC first flagged the company’s “gag clauses” prohibiting pharmacies from disclosing rebate information to patients. Over three years, the agency built a case anchored in monopolization and exclusionary conduct doctrines.
Central to the argument was “price-inflation through rebate recycling.” Express Scripts negotiated steep rebates from manufacturers, funneled portions back to large employers while keeping the remainder as profit, effectively inflating list prices that independent pharmacies had to accept. The FTC’s official docket contains over 2,500 pages of internal emails showing senior executives discussing “leveraging rebate flow to pressure small-shop pharmacies into silence.”
When the case reached the commission, the three-vote majority hinged on an analogy from FTC Chair Lina Khan: “Imagine a farmer who sells his wheat to a single grain elevator that decides, on a whim, how much to pay for each bushel. The farmer has no alternative market, and the elevator can dictate terms that keep the farmer from staying in business.”
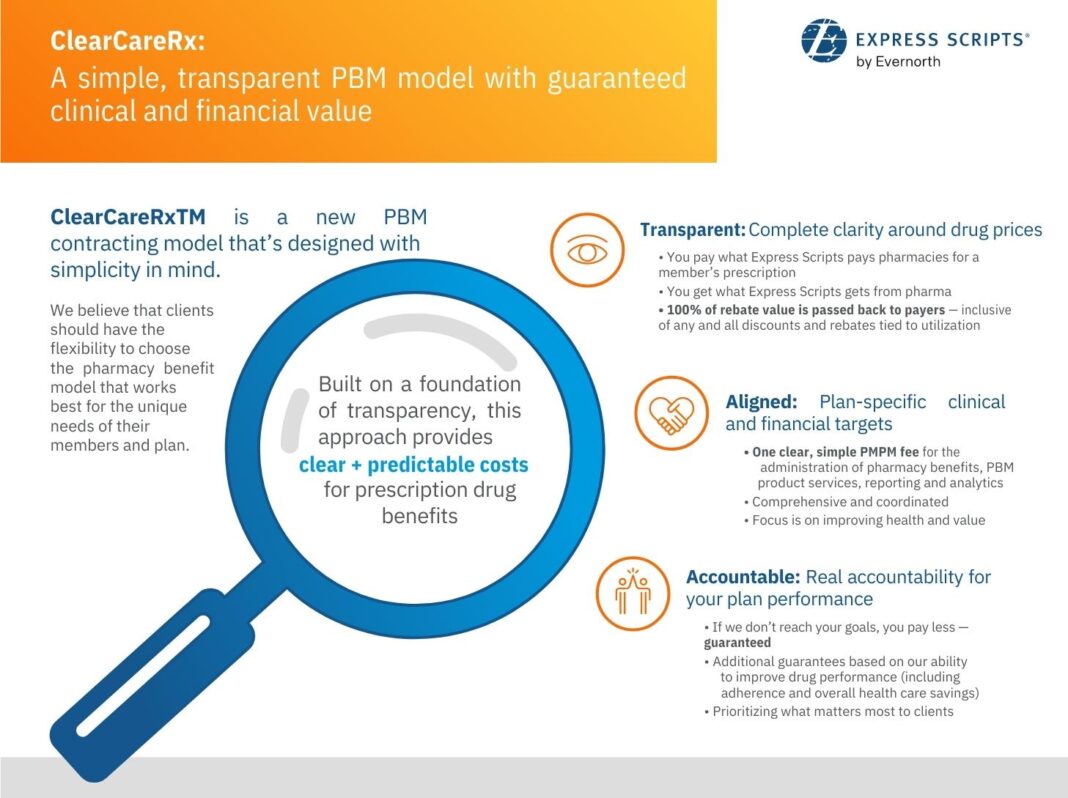
Critics argue the FTC overstepped, claiming the ruling could stifle innovation in drug-cost management. However, the commission’s decision includes a nuanced carve-out: PBMs may continue operating under a “transparent pricing” framework that requires real-time disclosure of rebates, administrative fees, and net drug costs to both employers and pharmacies.
Charting the Future: Emerging Models That Could Replace the Old PBM Paradigm
With Express Scripts’ model now on thin ice, the industry is experimenting with alternatives promising both cost containment and fairness. Two concepts have gained traction:
- Pharmacy-centric networks – Cooperatives of independent pharmacies pooling bargaining power to negotiate directly with manufacturers, bypassing traditional PBMs. Early pilots in Minnesota showed a 15% reduction in average wholesale price for generic drugs while preserving higher margins for participating pharmacies.
- Value-based contracts – Rather than basing reimbursement on volume, these agreements tie payment to clinical outcomes, such as reduced hospital readmissions for heart failure patients. A 2023 National Institutes of Health study found that value-based contracts saved Medicare $3.2 billion over two years.
Both approaches emphasize data transparency and patient outcomes over opaque rebate gymnastics. If the FTC’s enforcement continues pressuring the sector toward openness, we may witness rapid migration toward these models, especially as insurers scramble to meet new compliance benchmarks.
Transition challenges remain. Smaller pharmacies need technical support integrating electronic health record data with insurer platforms, and manufacturers must adjust pricing strategies that long relied on rebate leverage. Federal grants, such as the Health and Human Services “Pharmacy Innovation Fund,” are earmarked to help independent pharmacies upgrade their IT infrastructure—a crucial step toward leveling the playing field.
Looking Ahead: A Personal Take on the New Landscape
Standing beside Maria as she restocked shelves with fresh insulin pens, I felt history shifting. The FTC’s decision is not a panacea, but it represents a decisive crack in a wall that stood too long. The real test will be whether policymakers, insurers, and remaining PBMs can translate this legal victory into a sustainable ecosystem where patients receive affordable medication, pharmacists retain professional autonomy, and the market rewards genuine innovation rather than hidden rebates.
For countless neighborhoods relying on local pharmacists not just for pills but for counsel, reassurance, and familiar smiles, the ban on Express Scripts’ model offers a glimpse of a more equitable future. It reminds us that when monopolistic control recedes, community hands can step forward—steady, compassionate, and ready to heal.